
NOT FOR REPRINT
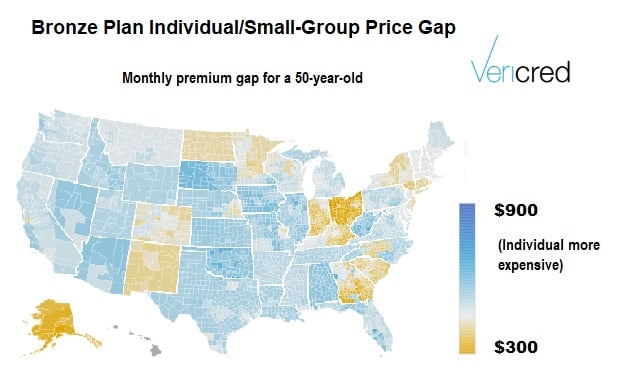
Some State Health Markets Tilt More Toward ICHRAs: Vericred
By
Allison Bell
News January 08, 2020 at 07:15 PM
Share & Print
NOT FOR REPRINT
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to asset-and-logo-licensing@alm.com. For more information visit Asset & Logo Licensing.